Aligning Incentives with Mission
There are a multitude of reasons a physician organization may consider a change in compensation structure for its providers. One significant consideration is whether the financial incentives contained within the compensation plan align with the overall mission and objectives of the organization. This article details two examples of how modifying the provider compensation structure can drive necessary changes in behavior that result in significant improvements.
Case Study #1
Our firm was engaged by a publicly funded Community Mental Health Center to revamp its physician compensation program. Due to financial constraints, physician compensation had remained unchanged over the last five years and as a result, physicians were upset at receiving below market compensation and physician productivity was beneath market benchmarks. This posed a significant challenge to our client as their mission is to provide accessible care to underserved patients in their community. The current situation threatened a vulnerable patient community’s access to care.
Using detailed billing records, call coverage shift calendars, and multiple interviews with administrative and physician leadership, we identified a prioritized listing of physician services and desired performance metrics. Variables in the compensation plan included work RVUs, call coverage shifts, encounters, base salary levels, and administrative compensation. Compensation drivers were tailored to the specific care venues – an emergency psychiatric center, the county jail, and outpatient clinics. With each scenario, we were able to quantify each physician’s compensation related to specific services, while providing administration a system-wide view of financial and mission impact.
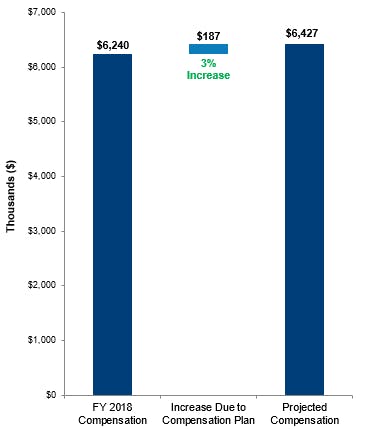
Through this customized process, we designed a compensation plan that was intended to be both fair to the physicians and budget neutral. High performing physicians were rewarded as appropriate, while lower performers received pay commensurate with their contribution to the organization. The plan put the client’s compensation program at market levels, for both compensation and productivity. In addition, our work uncovered important operational issues that were an impediment to physician productivity. These issues included poor patient throughput, proper electronic medical record utilization, and coding compliance and education.
"...we designed a compensation plan that was intended to be both fair to the physicians and budget neutral."
As a result of our work, physician productivity increased 17%. This is the equivalent of 4 FTEs of work based on historical productivity. This increased productivity will allow the center to achieve its mission of patient care in a more cost-effective manner by reducing the use of outside temporary physician staffing to meet patient needs.
Table 1: wRVU Comparison: Productivity Increase
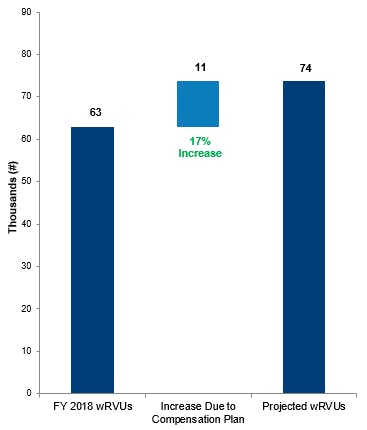
Table 2: Compensation Comparison: Budget Neutral
Case Study #2
Our firm was engaged by a physician group that was wholly-owned by a hospital. Our client was a multispecialty group and employed 200+ physicians, and their mission was to provide access to care to the underserved population of their community.
Due to their old compensation plan structure, there were subgroups of physicians that were not seeing enough patients, and there were other subgroups that were very productive, but not being paid at market levels for their services. The physician resource was not being deployed in an optimal manner, and the compensation structure was not aligned with the entity’s mission to serve the underserved.
Developing the Productivity Plan
First, we identified a common set of imperatives that aligned with the entity’s mission as it related to the compensation plan. These imperatives were:
- Incentivize work efforts independent of payor mix
- Employ quality metrics to reward high quality care
- Be economically sustainable
- Incorporate market-based (benchmark) data
- Be administrable
- Consistent with Fair Market Value
Through multiple meetings and iterations with a group of physician leaders and administration, we designed a productivity compensation plan that aligned the physician resource with the mission of the health system. We reviewed and used the following items as drivers of compensation:
- Productivity – work RVU production
- Call arrangements with the hospital - these included restricted call: STEMI, Labor and Delivery, and Critical Care, and restricted call for the hospitalist group
- Academic time – didactic teaching, supervising residents, and chair time
- Administrative time – medical directors
- Mid-level supervision
- Full-time equivalents (“FTEs”) – partial FTE providers had adjusted compensation plan metrics
- Quality / Outcomes
"...we designed a productivity compensation plan that aligned the physician resource with the mission of the health system."
Utilizing detailed billing records, full-time equivalent information, medical director and academic chair duties, call coverage shift calendars, and multiple interviews with administrative and physician leadership, we identified a prioritized listing of physician services and desired production metrics. In each calculation, we were able to quantify each physician’s compensation related to specific services, while providing administration a system-wide view of financial and mission impact. The compensation plan we developed required multiple iterations as a result of physician and leadership feedback, which we were able to adeptly and quickly quantify at both an individual and entity level. Ultimately, we developed an “at risk” wRVU productivity model for the specialists, who were more productive, and a “base + wRVU productivity” model for the primary-care physicians. In conjunction with leadership, we held a series of town hall meetings where we explained proposed compensation plan to physicians. These meetings were held to inform the physicians.
As a result of our work, physician productivity increased by 7% in year 1 of the compensation plan.
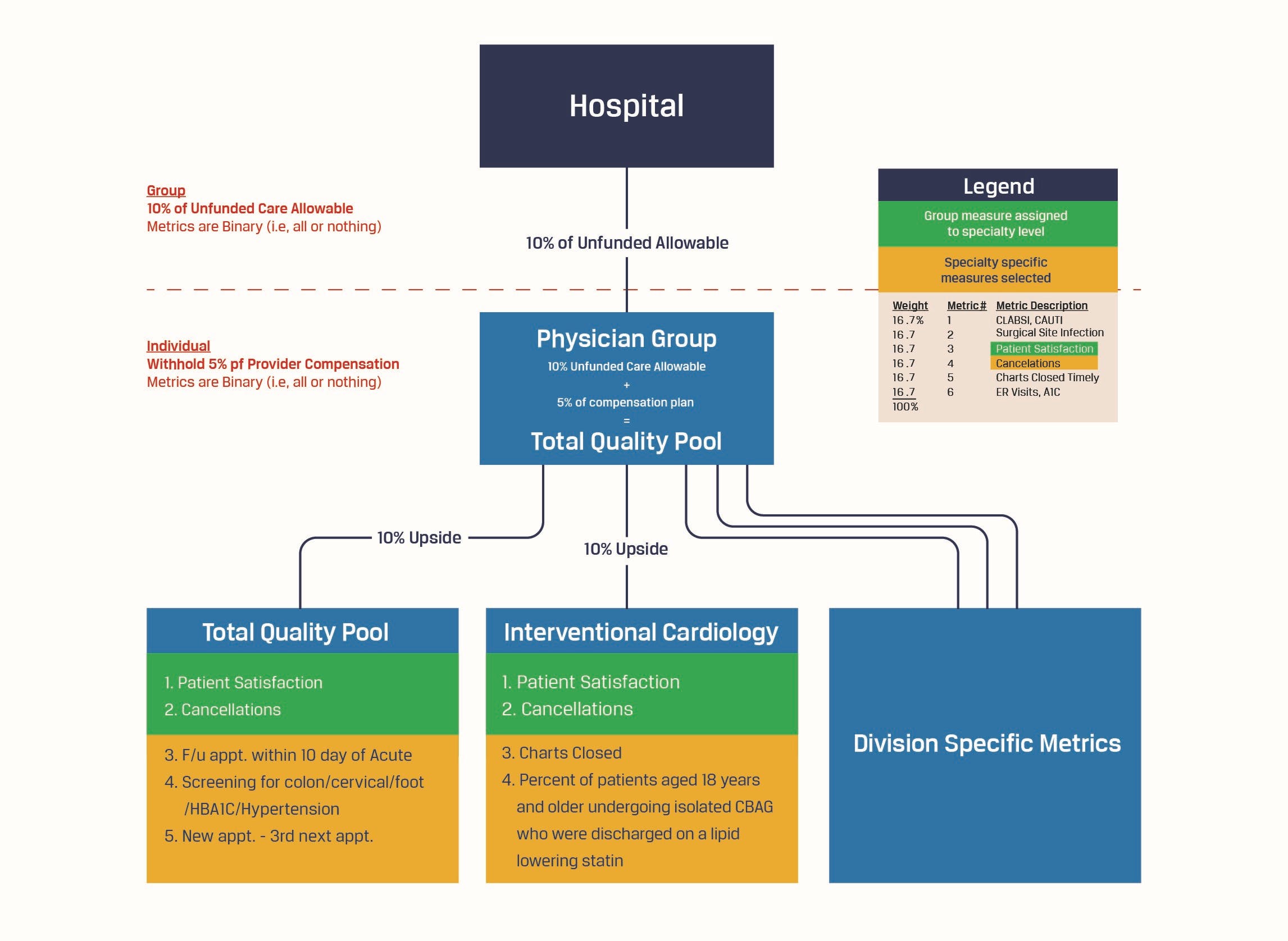
Quality Compensation Plan
A key component of the compensation plan related to quality and outcomes. The physician group had a set of key performance indicators (“KPIs”) that determined quality payments paid from the hospital to the physician group. (Examples of these KPIs are patient satisfaction surveys, hospital acquired conditions, surgical site infections, wait times, cancellation by physician). We developed a shared savings and risk model that held the physicians responsible for the metrics that they could influence. Again, through meetings with physician service-line leaders, we assigned 1-2 group KPIs to specific service lines and developed specific quality metrics that the specific specialty groups needed to focus on (for example, family medicine physicians were assigned a KPI of scheduling and performing a follow-up office visit within 10 days of an acute stay). We modeled the impact to each physician and were also able to show administration the potential risk and upside of implementing this portion of the compensation plan. The individual and quality bonus was contingent upon group adherence to the metrics.
Figure 1: Quality Compensation Model
In partnering with this entity, we implemented a plan that both increased physician productivity and moved the organization towards holding physicians accountable for quality outcomes. This plan ultimately aligned the entity with its mission to provide excellent care to the underserved population.
About the Authors
Anna Brewer, CVA
Partner - Director of Professional Development
817.546.7047
abrewer@jtaylor.com
As a Partner in the Consulting division, Anna leverages strong analytical and financial analysis skills in the areas of physician compensation, transaction support, valuations, due diligence, joint venture development, and strategic business plans. Her list of clients is comprised of physician practices, ambulatory surgery centers, community hospitals, multi-hospital systems, academic medical centers, and healthcare investors.
Garrett Gastil
Manager - Consulting Services
817.546.7044
ggastil@jtaylor.com
Since joining JTaylor in 2014, Garrett has gained experience in a breadth of practice areas allowing him to provide quality service and work products to his clients. He provides consulting and valuation services in various practice areas with an emphasis in the healthcare industry. Garrett’s fields of expertise include physician compensation, managed care contracts, transaction support, and mergers and acquisitions. There are a multitude of reasons a physician organization may consider a change in compensation structure for its providers. One significant consideration is whether the financial incentives contained within the compensation plan align with the overall mission and objectives of the organization. This article details two examples of how modifying the provider compensation structure can drive necessary changes in behavior that result in significant improvements.




